MENARINI is a fully integrated privately owned pharma company with a long and successful heritage in strategic partnering across the globe. We have a profound know-how stemming from our strong R&D capabilities in key therapeutic areas, coupled with our excellence in commercial execution and our powerful direct presence on a global basis.
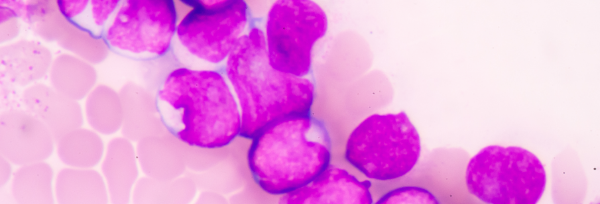
Acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS).
Acute myeloid leukemia (AML) is a cancer of the blood and bone marrow. AML accounts for nearly 80% of all adult acute leukaemias with an annual incidence of approximately 3.55 per 100,000 adults; its incidence increases progressively with age to greater than 20 per 100,000 adults aged 80 years or older. In contrast, AML accounts for 10% of childhood leukaemias with an annual incidence of less than 1 per 100,000 children. The median age at diagnosis is about 70 years. Most patients with AML present with signs and symptoms arising from bone marrow failure and organ infiltration by leukaemic cells. AML is a heterogeneous clonal disease characterized by recurrent genetic, epigenetic and metabolic abnormalities.
The prognosis of most patients is poor, with a 5-year survival of 28%, following conventional treatment. The outcome in older patients is even worse, with a median survival of less than 12 months.
Myelodysplastic syndrome (MDS) is a group of malignant blood disorders in which the bone marrow fails to produce healthy blood cells. Although the onset of a MDS before the age of 50 years is rare, the various subtypes of this disease are probably the most common cause of acquired bone marrow failure in older adults, among whom the annual incidence exceeds 75 per 100,000 persons. The median age of occurrence is about 70 years. The common presenting features relate to anaemia and other cytopenias. Dysplastic abnormalities in the bone marrow involving >10% of a specific myeloid cell lineage is the cardinal feature of MDS. The natural history ranges from indolent with a survival approaching that of the general population to subtypes with clinical outcomes not dissimilar to AML. There is evidence of immune dysregulation in some patients, which may cause autoimmune myelosuppression and worsen the ineffective hematopoiesis. Although the precise nature of the initiating event for MDS is unknown, much has been learned about the genomic landscape, abnormalities of the bone marrow microenvironment and how these features impact the natural history and some of the attributes of the clinical phenotype.
The remarkably heterogenous nature of MDS underscores the importance of a risk-adapted treatment strategy, informed by the revised-IPSS risk score and patient-related factors, such as age, performance status, frailty and co-morbidity. At present, allogenic HSCT is the only treatment that can offer long-term remission, but is not applicable for most patients, in view of age and comorbidities.